By now, I'm sure you've heard about the recent Medicare policy that aims to cut doctor payments for specialty procedures.
The headlines have been flying, physician groups are upset, and everyone seems to have an opinion about what this means for American healthcare. But what's actually going on here?
On November 1, 2025, just one day before the legal deadline, the Centers for Medicare and Medicaid Services (CMS) finalized the 2026 Medicare physician fee schedule. This policy was released during the government shutdown, after bringing furloughed workers back.
The new rule introduces what CMS calls an “efficiency adjustment” — a 2.5% cut to payments for over 7,000 medical services.
We're talking about surgeries, radiology services, pain management procedures, gastroenterology services, and more.
Basically, if it's a specialty procedure that involves more than just time spent with a patient, it's probably affected.
Now, Congress actually passed a 2.5% pay increase for doctors back in July as part of the “One Big Beautiful Bill.” So you might be thinking: doesn't that cancel out? Well, yes — that's exactly the point of contention.
Primary care doctors and services billed based on time (like therapy sessions or office visits) get to keep that raise. But specialists performing procedures? Their increase gets wiped out by this efficiency adjustment.
Doctors participating in alternative payment models will see a 3.77% overall increase, while those in traditional fee-for-service arrangements get 3.26%. But then subtract that 2.5% efficiency adjustment for procedures, and suddenly, specialists are looking at much smaller increases.
Or in some cases, actual cuts when you factor in other changes.
Image Source: AMA
Learn more: Medicare Physician Payment Cuts 2025: 2.8% Reduction Impact and What Doctors Need to Know
The Logic Behind the Medicare Specialty Care Cuts
CMS's argument is pretty straightforward: technology improves, workflows get smoother, and procedures that used to take an hour might now take 45 minutes.
Therefore, Medicare has been overpaying relative to the actual resources these services require today.
Medicare Director Chris Klomp put it this way: “CMS is reinforcing primary care as the foundation of a better healthcare system while ensuring Medicare dollars support real value for patients, and not the kind of waste or abuse that erodes trust in the system.”
He added that the goal is simple: “deliver better outcomes for patients and be wise stewards of the taxpayer resources that make Medicare possible.”
The Flipside
Here's where specialists push back. Dr. Patrick Giam, president of the American Society of Anesthesiologists, didn't mince words. “These CMS policies represent poor policy decisions that demonstrate CMS's unwillingness to listen to physicians who are under significant financial stress.”
A recent study found there hasn't actually been an efficiency gain in procedure times.
In fact, some procedures are becoming more complex and taking longer as patient populations age and arrive with more complicated conditions.
Think about it — are today's 75-year-olds presenting with the same health profiles as 75-year-olds did twenty years ago?
Dr. Qihui Zhai, president of the College of American Pathologists, made a similar point, arguing that “these reductions to physician work ignore the realities of modern medicine, including rising patient complexity and evolving technologies that demand more from physicians, not less.”
Dr. Gregory Nicola, chair of the American College of Radiology Commission in Economics, was even more direct in his assessment: the efficiency adjustment “is not based in modern care reality and is not helpful.”
So who's right? Are procedures getting easier, or are they getting more complicated? It seems like it might depend on which procedure we're talking about…and that's exactly the kind of nuance that gets lost in sweeping policy changes.
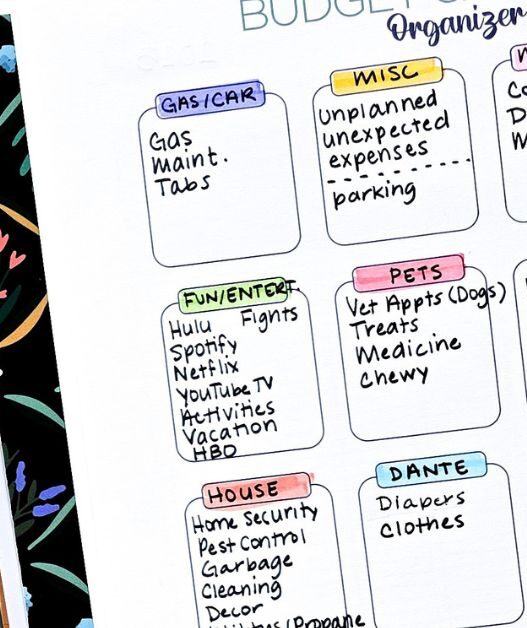
According to the American Medical Association's analysis, more than one-third of oncologists face cuts between 10% and 20% next year. We're talking about cancer doctors, i.e., people treating some of the sickest, most vulnerable patients in the system.
Meanwhile, 37% of obstetricians and gynecologists will see their reimbursement drop.
Other hard-hit specialties include radiology, gastroenterology, anesthesiology, and pathology.
In case you missed it: The Hippocratic Divide: How the “Beautiful Bill” Fractures American Healthcare
The Primary Care Perspective
On the other hand, primary care doctors are actually celebrating.
Ann Greiner, CEO of the Primary Care Collaborative, praised the policy as “an important step to address methods that have long diverted funding away from the whole-person, relationship-based primary care Americans need.”
The American Academy of Family Physicians also expressed satisfaction with the rule's prioritization of primary care.
Primary care has been undervalued in American healthcare for decades. We've created a system where a doctor who spends 45 minutes listening to a patient, coordinating their care across multiple conditions, and preventing future health problems gets paid less than one who performs a 15-minute procedure.
Primary care advocates argue that this imbalance has contributed to physician shortages in family medicine and pushed too many talented doctors toward more lucrative specialties.
The AMA's Diminishing Influence
There's another layer to this story that's fascinating if you're into healthcare policy (and let's be honest, if you've read this far, you probably are).
This rule represents a significant challenge to the American Medical Association's traditional power in setting Medicare rates.
For years, the AMA's committee has used surveys to estimate how long procedures take, how intense the work is, and what they should cost. CMS has grown increasingly critical of this process, arguing that the surveys are subjective, have low response rates, and create conflicts of interest since doctors have financial incentives to inflate how difficult their work is.
AMA President Dr. Bobby Mukkamala responded to the changes by urging CMS “to base policy changes on verifiable data, including results from the Physician Practice Information Survey,” — which seems reasonable enough.
But what counts as verifiable data in this context? CMS thinks the current survey system is flawed. The AMA thinks CMS's assumptions about efficiency gains are flawed. How do we break that stalemate?
The AMA also raised concerns about another aspect of the rule, with Mukkamala noting that “private practices across the country are expressing concern this rule would further put them at a disadvantage merely for treating patients at a hospital or ambulatory surgery center.”
He added that “As the new rule is implemented and its changes are felt, we will share with CMS the real-world impacts — data and details not always easily available to policymakers in Washington. This exchange and collaboration are vital to keeping practices open during a physician shortage.”
The Budget Neutrality Trap
Here's the thing that makes all of this even more complicated: Medicare physician payments are required by law to be budget neutral. That means if one group of doctors gets a raise, another group has to take a cut. It's a zero-sum game.
This creates inevitable tension between specialties. Primary care physicians get an increase, specialists face cuts.
Congress could change this by tying Medicare increases to inflation without requiring offsets, but that would cost additional federal money. In our current political climate, good luck with that.
The Medical Group Management Association pointed out that the rule doesn't make up for years of underfunding or provide future sustainability for physicians.
Anders Gilberg, the organization's senior vice president of government affairs, warned that the final fee schedule “includes many policies that will threaten the financial sustainability of medical groups and cause significant disruption to their operations.”
So should we be forcing different types of doctors to compete for the same pot of money, or should we be growing that pot to adequately compensate everyone?
The Skin Substitute Situation
While we're talking about Medicare spending, there's another wild part of this story. The rule also addresses skin substitutes — those high-tech bandages used in wound care.
Medicare spending on these products exploded from $256 million in 2019 to over $10 billion in 2024. That's a nearly 40-fold increase in five years.
CMS says providers have been pushing these products without clear evidence that they work better than cheaper alternatives, sometimes just to drive profits. Starting in 2026, they're reclassifying how they pay for these products, which will cut spending by almost 90%, saving nearly $20 billion next year.
The companies that make these products lobbied hard against this change. They lost. What does that tell us about where CMS is willing to draw the line on spending?
What About Telehealth?
The Medicare Specialty Care rule also makes some consequential decisions about virtual care.
CMS is lifting frequency limits on virtual care in hospitals and allowing teaching physicians to supervise residents over video. Both moves expand access and improve medical education.
But there's a catch.
After 2025, doctors won't be able to bill Medicare for after-hours telehealth visits they perform from home. If you've ever had a doctor answer your question via a video call at 8 PM because you were worried about symptoms, that's the kind of convenience that might become harder to access.
Changes to Medicare: What 2025's Overhaul Really Means for Your Care
Frequently Asked Questions
What is the Medicare efficiency adjustment for 2026?
The Medicare efficiency adjustment is a 2.5% payment cut affecting over 7,000 specialty services starting in 2026. It applies to procedures like surgeries, radiology, pain management, and gastroenterology. CMS argues that technology and improved workflows have made these procedures more efficient, so Medicare has been overpaying. However, specialists dispute this, citing research showing procedures haven't become more efficient.
Which doctors are affected by the Medicare payment cuts?
Specialty physicians performing procedures are most affected. The AMA reports that over one-third of oncologists face 10–20% cuts, while 37% of OB-GYNs will see reduced reimbursement. Other hard-hit specialties include radiology, gastroenterology, anesthesiology, and pathology. Primary care physicians billing for time-based services will see payment increases instead.
Are all doctors getting a Medicare pay cut in 2026?
No. Congress passed a 2.5% increase in July 2025, which primary care doctors keep. Specialists performing procedures have their increase offset by the 2.5% efficiency adjustment. Doctors in alternative payment models see 3.77% increases overall, while traditional fee-for-service doctors get 3.26%, but specialists must subtract the efficiency cut.
Why is CMS cutting payments to specialty doctors?
CMS claims procedures have become more efficient due to technology, so payments should reflect lower resource requirements. The agency also wants to rebalance payments toward historically undervalued primary care. However, specialists argue that aging, more complex patients actually make their work harder, and recent studies show no efficiency gains in procedure times.
What is the Medicare physician fee schedule?
The Medicare physician fee schedule determines how much Medicare pays doctors for services. It's updated annually and covers over 10,000 services using a formula with relative value units (RVUs) and conversion factors. By law, updates must be budget neutral, meaning increases for some doctors require cuts to others.
Will the Medicare cuts affect patient care quality?
Specialists worry reduced payments could force them to see more patients in less time, potentially affecting quality. They're also concerned about affording the latest equipment with lower revenues. Some practices may close or merge with hospitals. Primary care advocates counter that better-funded primary care improves overall outcomes through prevention and care coordination.
What is Medicare's budget neutrality requirement?
Budget neutrality is a legal mandate that annual fee schedule updates can't increase overall Medicare spending. If one group of physicians gets higher payments, another must receive offsetting cuts. This zero-sum framework creates tension between specialties. Congress could eliminate it by tying increases to inflation, but that requires additional federal funding.
How does the AMA influence Medicare payment rates?
The AMA's committee traditionally uses physician surveys to estimate procedure time, intensity, and costs, heavily influencing CMS decisions. The 2026 rule reduces this influence, with CMS criticizing surveys as subjective with low response rates and conflicts of interest. The new policy “rebalances the approach” by relying less on physician self-reporting.
What are Medicare skin substitutes and why are payments changing?
Skin substitutes are high-tech wound care products. Spending exploded from $256 million (2019) to over $10 billion (2024). CMS says providers push these products without evidence they work better than cheaper alternatives. Starting 2026, Medicare reclassifies them as supplies rather than biologicals, cutting spending by 90% and saving $20 billion annually.
How will Medicare telehealth coverage change in 2026?
Mixed changes: CMS is lifting frequency limits on virtual hospital care and allowing teaching physicians to supervise residents via video. However, doctors can no longer bill Medicare for after-hours telehealth visits from home after 2025, potentially reducing convenient access to evening video consultations.
What is the WISeR Model in Medicare?
WISeR (Wasteful and Inappropriate Service Reduction) is an AI-powered program testing prior authorizations in six states starting January 1, 2026. It uses machine learning to manage approvals for Medicare fee-for-service. Key details remain unknown due to the government shutdown, and providers are calling for delays.
Which states will be affected by Medicare payment changes?
The efficiency adjustment and fee schedule changes apply nationwide to all doctors treating Medicare's 65+ million beneficiaries. However, specific programs like the WISeR Model will initially launch in only six states (not yet specified due to the government shutdown).
How do alternative payment models affect Medicare reimbursement?
Alternative payment models (APMs) tie compensation to quality and cost outcomes rather than service volume. Under 2026 rules, doctors in qualifying APMs get 3.77% conversion factor increases versus 3.26% for traditional fee-for-service — a three-fold difference designed to incentivize value-based care over volume.
Will primary care doctor shortages improve with these changes?
Primary care advocates hope so. They argue decades of undervaluing primary care pushed medical students toward lucrative specialties. Higher reimbursement could make primary care more attractive financially. However, whether this shifts specialty choices or reduces shortages remains uncertain, and critics say changes may not be substantial enough.
What happens to private medical practices under the new Medicare rules?
Private practices, especially specialty ones, face increased financial pressure from the efficiency adjustment and facility-based service payment cuts. The AMA notes practices worry the rule puts them “at a disadvantage.” These pressures may accelerate closures or hospital acquisitions, continuing healthcare consolidation trends.
Can Congress override the Medicare payment cuts?
Yes. Congress regularly intervenes to prevent cuts, most recently passing the 2.5% increase in July 2025. However, the efficiency adjustment comes from CMS regulatory authority. While physician groups will lobby for relief, any legislative fix requires political will and additional funding to avoid budget neutrality, which may be challenging.
How accurate are efficiency assumptions for medical procedures?
Highly contested. CMS argues technology makes procedures more efficient, justifying lower payments. However, recent research found no efficiency gains. Some procedures take longer due to aging, complex patients and evolving technologies. The disagreement highlights difficulty in objectively measuring medical work complexity and efficiency.
What does this mean for Medicare beneficiaries?
Impact is uncertain and mixed. Primary care advocates say proper funding improves preventive services and outcomes. Specialists warn cuts could affect specialty access, especially in rural areas. Some doctors may see more patients in less time, potentially affecting appointment quality. The rule could also accelerate practice consolidation, changing where beneficiaries receive care.
When do the Medicare payment changes take effect?
All changes — efficiency adjustment, skin substitute payment changes, telehealth modifications, and new payment rates — take effect January 1, 2026. The WISeR Model also launches the same date in six states, though implementation details remain unclear due to the government shutdown. Providers have limited preparation time.
What is the “One Big Beautiful Bill” and how does it affect Medicare?
The “One Big Beautiful Bill” is GOP tax and spending legislation passed in July 2025, mandating a 2.5% one-year pay increase for physicians treating Medicare beneficiaries. This congressional increase reversed multiyear reimbursement cuts. However, CMS's efficiency adjustment cancels out this raise for specialty procedures, creating major controversy in the medical community.











![How to Watch MeTV Without Cable [Stream MeTV Live]](https://rjema.com/wp-content/uploads/2025/12/How-to-Watch-MeTV-Without-Cable-Stream-MeTV-Live-527x630.jpg)
![How to Get Free Cable TV [Free TV Legally]](https://rjema.com/wp-content/uploads/2025/12/How-to-Get-Free-Cable-TV-Free-TV-Legally-527x630.jpg)